| ||||
Can Changing Weather Make a Person Sick?
from Science Prof Online
Regardless of whether it is the common cold, flu, plague or something as simple as an abscess, a person can only become ill from infection after being exposed to an infectious agent, such as a virus, bacterium or eukaryotic microbe. Without the involvement of some type of pathogen (disease causing microbe), a person cannot develop an infection.
However beyond this simple point, the factors that can affect disease-based illness become a bit more complicated.
Article Summary: Whenever there is a sudden change in the weather, complaints of illness abound; old wives tale, or is there really a link between infection and climate?
Can Changes in the Weather Make You Sick?
 | ||||
You have free access to a large collection of materials used in a college-level introductory microbiology course. The Virtual Microbiology Classroom provides a wide range of free educational resources including PowerPoint Lectures, Study Guides, Review Questions and Practice Test Questions.
Page last updated: 6/2014
SCIENCE PHOTOS
SPO VIRTUAL CLASSROOMS
 | ||||||
SPO is a FREE science education website. Donations are key in helping us provide this resource with fewer ads.
Please help!
(This donation link uses PayPal on a secure connection.)
Effect of Climate on the Immune System
The human immune system is what defends the body against infectious disease, and this immunity-related collection of physical structures, cells, chemicals and processes are enormously complicated. Since the immune system is so complex, there are many factors that can affect how it functions, including genetics, physical and psychological stress, illness and even climate. Hypothermia (lowering of core body temperature) is just one example of a climate-related factor that has been shown to impair immune response.
In addition to climate impacting immune function, changes in the weather can impact the behavior of infectious agents themselves, the animal hosts that help spread disease, the people who may become infected.
The Effect of Climate on Infectious Agents
Influenza is a cold weather illness. This is because the influenza virus is transmitted through airborne respiratory droplets that have been introduced into the air through coughs and sneezes. When a person who has influenza coughs or sneezes, her or she propels numerous influenza viruses onto the surrounding air which the people around them can breathe in.
Influenza viruses can only remain airborne in atmospheric conditions of low humidity, common in colder months. When humidity increases, water molecules in the atmosphere cling to airborne flu viruses and cause them to drop to the ground, where they cannot be breathed in.
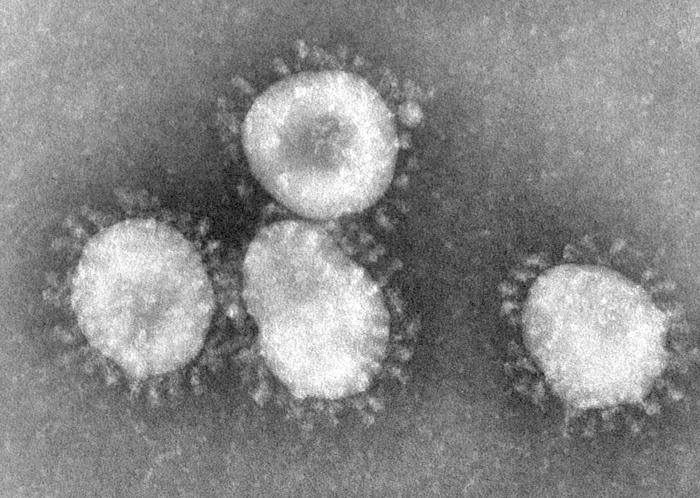
Coronaviruses are one type of virus known to cause the common cold. They have a halo, or crown-like (corona) appearance when viewed under an electron microscope.
For more information on influenza and vaccination, check out >
"What You Should Know for the 2013 - 2014 Influenza Season", from the CDC
and
Find out why Joe Thomas of the Cleveland Browns gets his seasonal influenza vaccine.
Climate, Human Behavior and Infectious Disease
In contrast, the viruses that cause the common cold are transmitted largely through contact—by a person touching an object with the virus on it and then touching his or her eyes, nose or mouth. Locations or times of year in which people are more prone to congregate indoors, in close contact, will promote the spread of cold viruses.
Effect of Climate and Environment on Vectors of Infection
A vector is an organism that can carry and spread infectious agents, and sometimes the relationship between host, vector and microbe can be rather complex. For example, Yersenia pestis is the bacterium that causes bubonic and pneumatic plague. It is spread when the fleas of rats bite humans. Sanitation, food and water conditions have a huge impact on the rat population, which has an effect on the flea population, which therefore impacts the prevalence of plague.
There are also many diseases that are mosquito-borne. Diseases such as West Nile virus and malaria are cause by microbes, and distributed when mosquitoes carrying the virus bite a human. Moisture levels in the environment impact the prevalence of these diseases by impacting the population of mosquitoes.
Allergies, Asthma & Illness
Allergies and asthma can also be aggravated by changes in the seasons and the weather, and those with preexisting respiratory issues are particularly vulnerable to respiratory infections. Although to develop an infection, a person must be exposed to an infectious agent, preexisting respiratory conditions can made it easier for an infection to develop and worsen when someone with allergies of asthma is exposed to disease-causing microbes.
Sources & Resources
- Bauman, R. (2014) Microbiology with Diseases & Taxonomy 4th ed., Pearson Benjamin Cummings.
- Gosai,A., Salinger, J. & Dirks, K. (2009) "Climate and Respiratory Disease in Auckland, New Zealand", Australian and New Zealand Journal of Public Health, Vol. 33, Iss. 6; pg. 521
- Russwurm S. et al (2004) "Direct Influence of Mild Hypothermia on Cytokine Expression and Release in Cultures of Human Peripheral Blood Mononuclear Cells". Journal of Interferon & Cytokine Research. February 2002, 22(2): 215-221.
- Tang, J.et al (2010) "Incidence of Common Respiratory Viral Infections Related to Climate Factors in Hospitalized Children in Hong Kong". Epidemiology and Infection, Vol. 138, Iss. 2; pg. 226.
- Tortora, G., Funke, B., Case, C. (2010) Microbiology, an Introduction. Benjamin Cummings.